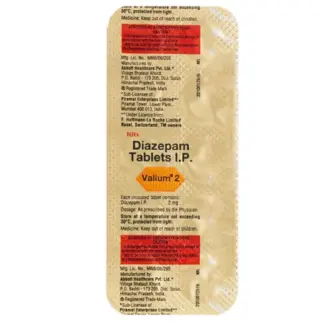
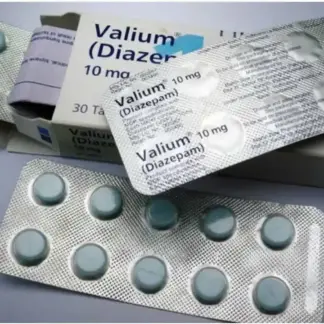
Diazepam and Valium are two names that are often used interchangeably, but it’s crucial to understand that they refer to the same medication. Valium is the brand name for the drug diazepam, a widely prescribed benzodiazepine that acts as a central nervous system (CNS) depressant. This medication is commonly used to treat anxiety disorders, alcohol withdrawal symptoms, muscle spasms, and other conditions. In this my-tramadol.com article, Read the intricacies of diazepam/Valium, its mechanism of action, uses, side effects, and potential interactions.
What is Diazepam And Valium?
Diazepam, also known as Valium, belongs to the benzodiazepine class of drugs, which work by enhancing the effects of gamma-aminobutyric acid (GABA), a neurotransmitter that inhibits brain activity. By increasing GABA’s effects, diazepam/Valium produces a calming, sedative, and muscle-relaxing effect. This medication is one of the most commonly prescribed benzodiazepines due to its long half-life, which means it remains in the body for an extended period.
Indications and Uses
Diazepam/Valium is approved for various medical conditions, including:
- Anxiety Disorders: It is widely used to treat generalized anxiety disorder, panic disorders, and other anxiety-related conditions.
- Alcohol Withdrawal Symptoms: Diazepam/Valium can help alleviate the symptoms associated with alcohol withdrawal, such as tremors, insomnia, and seizures.
- Muscle Spasms and Spasticity: Due to its muscle-relaxant properties, diazepam/Valium is sometimes prescribed to treat muscle spasms and spasticity caused by conditions like multiple sclerosis or spinal cord injuries.
- Seizure Disorders: In some cases, diazepam/Valium may be used as an adjunctive therapy for certain types of seizure disorders.
- Pre-operative Sedation: Diazepam/Valium can be administered before surgical procedures to induce relaxation and reduce anxiety.
Mechanism of Action and Effects
Diazepam/Valium exerts its effects by binding to specific receptors in the brain and enhancing the activity of GABA, the primary inhibitory neurotransmitter in the central nervous system. This action leads to a decrease in neuronal excitability, resulting in a calming, sedative, and muscle-relaxant effect. The effects of Valium can include:
- Reduced Anxiety and Stress: Diazepam/Valium can help alleviate the physical and psychological symptoms of anxiety, such as restlessness, muscle tension, and excessive worry.
- Muscle Relaxation: Due to its muscle-relaxant properties, diazepam/Valium can help relieve muscle spasms, cramps, and stiffness.
- Sedation and Sleep Induction: At higher doses, diazepam/Valium can induce sedation and promote sleep, making it useful for managing insomnia.
- Anticonvulsant Effects: Diazepam/Valium can help prevent or control certain types of seizures by increasing the seizure threshold.
Common Side Effects and Precautions
Like other benzodiazepines, diazepam/Valium can cause various side effects, some of which may be more pronounced with higher doses or long-term use. Common side effects include:
- Drowsiness and Sedation: Diazepam/Valium can cause excessive sleepiness, fatigue, and impaired coordination, which may affect daily activities and increase the risk of accidents.
- Cognitive Impairment: Memory problems, confusion, and difficulty concentrating are potential side effects of diazepam/Valium.
- Dizziness and Vertigo: Some individuals may experience dizziness, vertigo, or a feeling of unsteadiness while taking diazepam/Valium.
- Respiratory Depression: In rare cases, diazepam/Valium can cause respiratory depression, especially when combined with other CNS depressants or taken in higher doses.
- Dependence and Withdrawal: Long-term use of diazepam/Valium can lead to physical and psychological dependence, and abrupt discontinuation may result in withdrawal symptoms.
It’s essential to use diazepam/Valium under medical supervision and follow the prescribed dosage and duration to minimize the risk of side effects and dependence.
Drug Interactions and Contraindications
Diazepam/Valium can interact with various medications, including:
- CNS Depressants (e.g., alcohol, opioids, barbiturates): Combining diazepam/Valium with other CNS depressants can lead to increased sedation, respiratory depression, and potentially life-threatening complications.
- CYP3A4 Inhibitors/Inducers: Drugs that inhibit or induce the CYP3A4 hepatic enzyme can affect the metabolism and elimination of diazepam/Valium, potentially leading to increased or decreased effects.
- Oral Contraceptives: Diazepam/Valium may increase the risk of breakthrough bleeding or contraceptive failure when taken with oral contraceptives.
- Antidepressants: Some antidepressants, such as fluoxetine (Prozac), can increase the risk of toxicity when combined with diazepam/Valium.
It’s crucial to inform your healthcare provider about all medications, supplements, and existing medical conditions before starting diazepam/Valium to avoid potentially harmful interactions.
Long-term Use and Dependence
While diazepam/Valium can be an effective short-term treatment for various conditions, long-term use carries the risk of physical and psychological dependence. Prolonged use can lead to tolerance, where higher doses are required to achieve the desired effects. Additionally, abrupt discontinuation of diazepam/Valium after long-term use can result in withdrawal symptoms, which may include:
- Anxiety and Irritability
- Insomnia and Nightmares
- Muscle Cramps and Tremors
- Seizures (in severe cases)
To minimize the risk of dependence and withdrawal, it’s essential to follow the prescribed dosage and duration and consult with a healthcare professional before discontinuing diazepam/Valium.
Comparison of Diazepam and Valium:
| Characteristic | Diazepam | Valium |
| Drug Class | Benzodiazepine | Benzodiazepine |
| Brand Name | N/A | Valium |
| Generic Name | Diazepam | Diazepam |
| Mechanism of Action | Enhances the effects of GABA, leading to sedation, muscle relaxation, and reduced anxiety. | |
| Indications | Anxiety disorders, alcohol lead to withdrawal, muscle spasms, seizure disorders, pre-operative sedation. | |
| Side Effects | Drowsiness, cognitive impairment, dizziness, respiratory depression (rare), dependence, and withdrawal. | |
| Drug Interactions | CNS depressants, CYP3A4 inhibitors/inducers, oral contraceptives, antidepressants. | |
| Long-term Use | Risk of physical and psychological dependence, tolerance, and withdrawal symptoms. | |
| Any Discount To Purchase Online? | Yes, Buy Diazepam Online | Buy Valium Online |
Conclusion
Diazepam and Valium are two names that refer to the same medication, a widely prescribed benzodiazepine used to treat various conditions, including anxiety disorders, alcohol withdrawal symptoms, muscle spasms, and seizure disorders. While diazepam/Valium can be an effective treatment option, it’s essential to understand its mechanism of action, potential side effects, drug interactions, and the risks associated with long-term use and dependence. Proper medical supervision, adherence to prescribed dosages, and awareness of potential complications are crucial for safe and effective use of